Dr. Felipe Teran, MD (@FTeranmd), Faculty and Fellow in the Divisions of Emergency US and Emergency Critical Care at Mount Sinai, Co-Director of the Resuscitate NYC 2017 EMCrit Conference, discusses the role of ultrasound in cardiac arrest (02/08/2017).
Conference
Grand Rounds: Airway
Dr. Pik Mukherji, MD (@ercowboy) of Northwell Health, LIJMC Program Director presents on Airway Management (03/08/2017)
Grand Rounds: Educating Your Patients
Dr. Teresa Y. Smith, MD, MSEd, Residency Program Director at SUNY Downstate/Kings County presents on educating our patients in the emergency department (09/14/2016)
Grand Rounds: Ocular POCUS
Dr. Andrew Shannon, MD, MPH of University of Florida College of Medicine – Jacksonville presents on Ocular Point-of-Care Ultrasound (POCUS) (07/20/2016)
Lecture Notes
- Up to 67% of periorbital fractures have associated ocular trauma
- Periorbital swelling may prevent traditional exam
- Medial area includes ducts that may require stents if violated in trauma
- Temporal region of internal anatomy includes optic disk and nerve; nasal includes fovea and macula
- Possible to evaluate for pupil diameter in axial cut under ultrasound
- Retina usually not visible on U/S
- Optic nerve sheath is visible on ultrasound, not the optic nerve
- Amount of energy required for temperature change in the retina is much less than that required to make a change at other tissue
- Avoid over-exposing
- Apply tegaderm as barrier prior to exam
- Complaint of
- “blurry vision”
- “wavy” visual loss
- curtain comes down/across vision
- Retina has blood supply from choroid
- As fluid accumulates between choroid/retina → retinal ischemia
- Retina is tethered to the choroid at the Ora Serrata and at the optic nerve
- If you see a detachment that does not respect the optic nerve, consider vitreous detachment instead of retinal detachment
- Worried about these in setting of trauma
- May be obscured by vitreous hemorrhage
- Retina will be hyperechoic and undulating
- May have vitreous hemorrhage + retinal detachment; can be detected on POCUS
- Sudden, painless, floaters, dark spots, flashes
- 2/2: Trauma vs DM vs sickle cell
- POCUS: Hyperechoic, clotted blood
- Looks like clothes in a washer
- Terson’s Syndrome
- Vitreous hemorrhage associated with ICH (SAH)
- Occurs in 13% of patients with SAH
- Posterior Vitreous Detachment
- May also appear as hyperechoic linear density “lifted off” posterior globe
- Thinner, smoother, darker than retinal detachment
- Crosses optic nerve (unlike RD)
- May present as diplopia and blurry vision
- Herniation of inferior rectus
- Compartment syndrome of the eye
- 90-120 min of ischemia → irreversible vision loss
- Tx: Timolol, pilocarpine, acetazolamide
- May require lateral canthotomy
- Indications: APD, loss of vision, IOP >40 mmHg
- May note extruded uveal tissue (almost always brown)
- Irregular pupil will point toward area of injury
- Pt NPO
- Abx: Cephalosporin or anti-penicillinase PCN (i.e. augmentin)
- Update tetanus
- Anti-emetic
- Shield eye & minimize manipulations
- Modified Seidel Test
- Use fluoroscein and cobalt blue filter to note aqueous humor flow
- Hyphema may be noted
- Ultrasound
- Avoid if unnecessary and use gingerly
- Findings
- ↓ in globe size
- AC collapse
- Buckling of sclera
- Anterior Chamber Decompression
- From trauma or eroding corneal ulcer
- Foreign Body
- May see in 30% of open globe
- Edge of lens may be visible in/through pupil
- Complete dislocation/luxation: Lens displaces into vitreous or rarely into AC
- Differential dx for monocular diplopia: lens dislocation vs psych
- Dislocation
- Posterior more often than anterior
- Typically s/p replacement (cataracts surgery); may see in Marfan’s and trauma
- Avoid dilating pupil
- ONS is contiguous with dura mater
- Papilledema is delayed in comparison to optic nerve sheath diameter change
- Normal ONS is up to 5.0 mm diameter
- Measure 3 mm posterior to globe for both eyes
- Take average 2 or more readings
- Average ONSD > 5.2 mm is considered abnormal
- Consider ↑ ICP
- If ONS <5 mm, unlikely ICP >20 mmHg
- If >5.8, suspect ↑ ICP
- Crescent sign: Optic nerve protrudes into the globe
- Drusen: Optic nerve head drusen; may falsely appear as a FB
Grand Rounds: Thrombolysis and Management of Acute Ischemic Stroke
Dr. Kathryn Kirchoff-Torres, MD of Montefiore Medical Center presents on Thrombolysis and Management of Acute Ischemic Stroke (07/20/16)
Grand Rounds: Pediatric Airway Management Update
Dr. Marianne Gausche-Hill, MD, FACEP, FAAP of Harbor-UCLA Medical Center presents on Pediatric Airway Management (06/22/16)
Biliary Tract Emergencies
Original lecture by Dr. Peter Gruber
Conference 1/27/2016
Post by Fernando Barajas Jacobi/Montefiore EM PGY-2

Cholelithiasis causes a spectrum of disease
The location of impaction along with the diseases associated with that are listed below. Each one has unique physical findings, laboratory findings, and imaging
(1)Gallbladder and cystic duct⟺biliary colic and acute cholecystitis
(2)Common bile duct, Common hepatic ducts ⟺ choledocholithiasis, cholangitis
(3)Sphincter of Oddi (or ampule of vater) ⟺gallstone pancreatitis
(4)Intrahepatic ducts ⟺ right, left, segmental hepatic ducts
(5)GI tract ⟺gallstone ileus
GALLBLADDER DISEASE
Historical clues and physical findings
- Traditionally (biliary) colic and acute cholecystitis (AC) were considered separate entities, however they are a spectrum of diseases***
- Pain often, but not always in the RUQ but can be epigastric
- Asymptomatic cholelithiasis/biliary colic (pain <5 hours)
- Colic—pain lasting less than 5 hours.
- May or may not be intermittent (vs constant)
- Postprandial pain intensification
- Moral of the story is not to rely on physical or lab findings for the diagnosis
- Always consider it in the Elderly; always consider it if the gallbladder is present
Epidemiology
- Yes: “fat females that are 40”
- Associated with HIV, gastric bypass (usually have ppx cholecystectomy), rapid weight loss
- Prevalence increases with age
Diagnosis: Imaging is a must
- US
- Gallstones with thickened wall or murphy’s= 98% PPV for AC
- GS w/o other findings = 99% NPV for AC
- HIDA
- Limited ability to delineate non-obstructive disease
- CT
- Is a must if you are considering complications of AC (gangrene, emphysematous AC)
- Often performed if US is NOT available

A: Pericholecystic fluid (arrow), stones, GBW thickening. B: CT of gangrenous AC with surrounding edema
Treatment
- NSAIDS
- Pain control
- may decrease risk of progression of colic to AC
- ABx recommended though AC not necessarily associated with infection
- There may be an increase risk of surgical site infection if antibiotics are given
- Acalculous AC
- 10-15% of AC, but primarily occurs in ICU
- Risk factors include prolonged feeding
- Along with emphysematous AC, these patient most likely to require cholecystectomy due to increased risk of perforation
ASCENDING CHOLANGITIS
Diagnosis
- Charcot’s triad (present in 50-70%)
- Often in the setting of choledocholithiasis
- If your patient has undifferentiated sepsis or altered mental status
- ↑ T. Bili +/- ↑ amylase, transaminases, alk phos
Imaging: Opposite of AC work up
- CT is 1st line because US has a sensitivity of 50% for choledocholithiasis
- ERCP is gold standard
- It allows for disempaction, BUT
- Has high complication rate, so it is often deferred
Treatment
- IVF, IVF, IVF
- Antibiotics
- Pressors as indicated
PANCREATITIS
Diagnosis
- Often requires 2 of 3: Abd pain, lipase >3x normal range, imaging
- Lipase elevation does not correlate with severity of disease
- Imaging:
- Perform a CT if there is worsening in clinical status, organ failure, or the diagnosis is unclear
- Defer 12-48hours as it is more helpful then
Treatment
- IVF
- Amount needed is controversial
- The goal is to decrease BUN & HCT to decrease risk of pancreatic necrosis
- If gallstone pancreatitis → perform ERCP
BILIARY TRIVIA
- Causes of Jaundice:

- Diagnosing Hepatitis B:

- General Liver Function Test factoids:
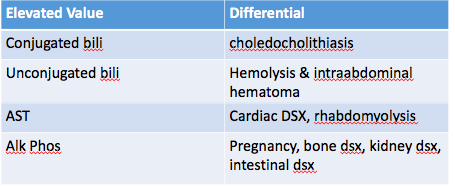
- If isolated derangement → extrahepatic
- If multiple derangements → liver disease
- GGT is the only lab that is specific for liver pathology
- With chronic injury
- LFTs are not sensitive and may even return to baseline
- If there was hepatic necrosis → ↑PT
- After resolution of disease → normalization of LFTs
- Transaminases
- AST/ALT >1
- Think alcoholic hepatitis
- AST, however, typical <500
- AST/ALT<1
- Think viral and toxic injuries
- Alk Phos
- If elevation >1000, consider metastatic CA
- AST/ALT >1
REFERENCES
Gruber PJ, et. al. Presence of fever and leukocytosis in acute cholecystitis. Ann Emerg Med. 1996 Sep;28(3):273-7.
Gruber P. “Biliary Tract Emergencies” Jacobi Medical Center. Jacobi/Montefiore Emergency Medicine Conference. Bronx. Jan 2016. Lecture
Tox Cases
- 52 yo M PMH type II DM BIBEMS after being found by wife unconscious.
- Initial FS 20. Given D50 in the field. Initial FS 20 in ED.
- Given additional amp D50 with improvement in MS but becomes obtunded 20 minutes later.
- Meds: Glyburide, glipizide, glimepiride
- Promotes pancreatic B-cell release of insulin through closing Katp channel/opening Ca channel → membrane depolarization → insulin vesicle exocytosis
- Glucose
- Important to understand caloric equivalent of interventions
- Amp D50 = 100 calories = 1 oreo
- D5 1/2 NS @ 250 mL/hr = 50 calories/hour = 1 ritz cracker/hour
- Give D10
- Give starchy food if tolerating PO
- Important to understand caloric equivalent of interventions
- Octreotide
- Blocks voltage dependent Ca channel → prevents insulin release
- Prevents recurrent hypoglycemia
- Consider in patients with inadequate response to dextrose
- 23 yo F with PMH HbSS, epilepsy p/w vertigo
- Difficulty ambulating over past 3 days, decreased visual acuity, dysarthria
- Patient in phenytoin and no history of overdose
- Symptoms dose dependent:
- Nystagmus (>15 mg/L)
- Ataxia (>30 mg/L)
- Lethargy (>50 mg/L)
- Mechanism of toxicity
- Inhibits post-synaptic Na channels → blocks burst of action potentials associated with seizures
- Cerebellum and hippocampus exhibit physiologic spontaneous neuronal burst activity
- Class 1b antiarrhythmic agent
- Case reports of bradydysrhythmias in patients taking medications that raise phenytoin levels
- Diluent
- Propylene glycol depresses myocardial tissue and decreases PVR
- Hypotension, dysrhythmias correlate with dose and rate of administration
- Loading dose should be given on cardiac monitor
- Inhibits post-synaptic Na channels → blocks burst of action potentials associated with seizures
- Treatment
- Mainly supportive
- Activated charcoal may be useful if <24h post-ingestion
- HD ineffective due to heavy-protein binding of phenytoin
- 42 yo M found unconscious, bradypneic following argument with girlfriend
- Empty bottle of Clonidine found in room
- VS: HR 50, BP 80/60, RR 8, O2 96%
- A: Alpha-2 agonists, antiarrhythmics
- B: Beta-blockers
- C: Calcium channel blockers
- D: Digoxin
- S: Sedatives, severe opioid toxicity
- Direct acting α2-adrenergic agonist
- Acts centrally and peripherally
- Central: Stimulates central α2-adrenergic receptors → inhibits catecholamine release in periphery → sedation and reduction of BP and HR
- Peripheral: Stimulates peripheral α2-adrenergic receptors on vascular smooth muscle → vasoconstriction
- Abuse
- Possesses opioid agonist properties at the μ-receptor
- Provides similar “nod effect” as heroin
- Typical dose for abuse: 1-3 mg PO
- Usually only seen in heroin/methadone abusers
- Supportive care
- Atropine
- IVF
- Theoretically, phenylephrine may be used if hypotension refractory to fluid resuscitation
- Ventilatory support as clinically warranted
- If severely hypertensive:
- May use nitro gtt
- Naloxone
- Some supporting evidence at case report and case series level
- May provide benefit if given early
- Minimal harm in opioid-naive patient
- 3 yo M BIB mom for lethargy
- Mom tried to wake him up this morning with difficulty
- No PMH; went to bed last night normal
- VSS, PERRL, skin exam normal, 2 mm sluggish pupils, diminished DTRs throughout, no e/o trauma
- Labs: Na 158, HCO3 7, Glucose 54, Ca 6.3, PO4 7.7, VPA level 801, AG 34
- Suppresses neuronal firing by blocking Na channels
- Increases GABA concentrations
- Metabolized by liver → elevations in LFTs and NH3 levels common
- Typically clinically insignificant at therapeutic VPA levels
- Class I antiarrhythmic; can affect QT
- Lethargy/cerebral edema
- Acute pancreatitis
- Fanconi’s syndrome (pediatrics)
- Heart block
- AKI
- Alopecia
- Coagulopathy
- Pancytopenia
- Optic nerve atrophy
- ARDS
- AG metabolic acidosis
- Hypocalcemia
- Hyperammonemia (metabolized in the liver)
- Hypoglycemia (compounded with sodium salts)
- Hypoglycemia
- Hyper/Hypophosphatemia
- Activated charcoal
- Hypotension
- IVF
- Pressors as necessary
- Consider HD
- Carnitine
- If associated hyperammonemia
- Hyperammonemia thought to be worsened in setting of carnitine depletion
- If associated hyperammonemia
- Naloxone
- Give if CNS and respiratory depression
- Minimal risk if patient not opiate dependent
REFERENCES
Chu, Jason. “Sulfonylurea agent poisoning.” Up To Date. http://www.uptodate.com, 03 Feb. 2016. Web. 12 Mar. 2016. http://www.uptodate.com/contents/sulfonylurea-agent-poisoning
Goldfrank, Lewis R. Goldfrank’s Toxicologic Emergencies. 9th Ed. New York: McGraw-Hill, 2011
Osterhoudt, Kevin. “Clonidine and related imidazoline poisoning.” Up To Date. http://www.uptodate.com, 29 Sep. 2014. Web. 12 Mar. 2016. http://www.uptodate.com/contents/clonidine-and-related-imidazoline-poisoning
Rivers, Colleen. “Valproic Acid Poisoning.” Up To Date. http://www.uptodate.com, 17 Apr. 2014. Web. 12 Mar. 2016. http://www.uptodate.com/contents/valproic-acid-poisoning
Su, Mark. “Phenytoin poisoning.” Up To Date. http://www.uptodate.com, 27 Oct. 2015. Web. 12 Mar. 2016. http://www.uptodate.com/contents/phenytoin-poisoning
Tintinalli, Judith E., and J. Stephan. Stapczynski. Tintinalli’s Emergency Medicine: A Comprehensive Study Guide. 7th ed. New York: McGraw-Hill, 2011.
Wellens’ Syndrome: A Cautionary Tale
Blog post based on an Evidence Based Medicine (EBM) discussion, January 20th, 2016.
Zwaan, C de, F W Bär, and H J Wellens. 1982. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. American heart journal
_____________________________________________________________
The Case:
Forty-nine year old M, no significant past medical history presents with chest pain that has since resolved. Started 3 hours ago (7pm) after refereeing a soccer game. Two episodes lasting maybe 15 minutes each. Pressure-like (places a closed fist over his chest when describing the discomfort), with questionable diaphoresis (after all, he had been running around), it does not radiate. No N/V or SOB. Prior to the game he had 3 cups of coffee and a large caffeinated ‘Monster’ energy drink, and attributes his pain to the energy drink. Is active and has never experienced this pain in the past. No cough or fever, no violent retching, no long car/plane travel or leg swelling, no trauma during the game he refereed.
Medications: none. Past Medical History: none. Past Surgical History: none. Social history: smoked cigarettes for a couple years as a teenager, but quit >25 years ago, and denies toxic habits including cocaine.
EXAM:
Vitals: T. 98.0, BP 129/98, HR 76, RR 18, O2 97% on room air
In no distress. Chatting with the nurse about all the coffee and Monster energy drink binged on. Skin warm, non diaphoretic.
No jugular venous distension
Heart rate regular, no murmurs, no POCUS performed
Lungs are clear, and he’s breathing comfortaby
No lower extremity edema, unilateral or otherwise
________________________________________________________________
10:30 pm (initial ECG)

04:24 (2nd ECG, 6 hours later), pain free. Scheduled as part of his rule out MI workup. He had been admitted, but was still in the ED.

_______________________________________________________________
Echo with Anterior wall motion abnormalities
Plan: Heparin gtt, Plavix, cath lab.
Cath lab: Large caliber, critical 95% mid LAD lesion, 2 drug eluting stents placed.
**Serial Trops negative
_______________________________________________________________

—-Zwann, Bar, Wellens et. al. American Hearth Journal 1982.
POPULATION: Non-randomized cohort of 145 patients in the Netherlands consecutively admitted because of impending myocadial infarction; defined as crescendo angina of recent onset, sudden worsening of recent angina, or crescendo post infarction angina developing after an initial asymptomatic period.
EXCLUSION: Patients with complete right bundle branch block, incomplete left bundle branch block, criteria for probable or definite left or right ventricular hypertrophy.
26/145 patients (18%) had unstable angina and the below ECGs.
**13/26 had these ECG findings on admission, the other 13 within 24 hours of admit.

Of those 26 patients with the above ECGs: 8 of first 9 suffered a massive anterior wall MI (prior to the realization of significance of ECG findings).
Uh oh!
In response, 10 of the next 17 were taken to the cath lab (of the 7 who were not; 2 were deemed too old to tolerate the procedure and 5 refused), plus the 1 patient from the first 9 who hadn’t had an MI. Eleven total. Take note of the column on the right, 10 patients had a critical Left Anterior Descending (LAD) stenosis, and 1 had a prolapsed mitral valve.
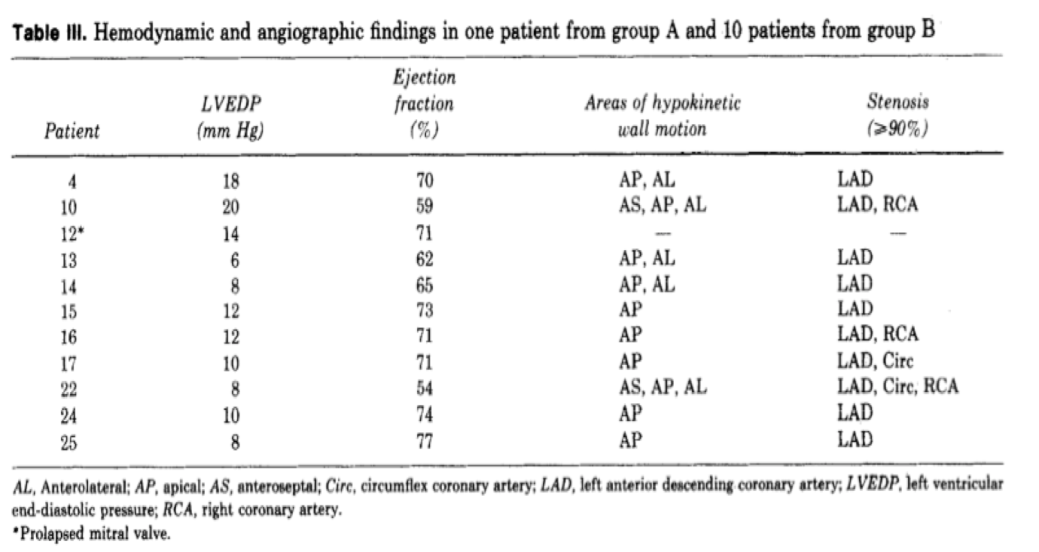
_____________________________________________________________
This piqued interest and in a follow-up prospective study in 1989 with 1260 unstable angina patients, 180 (14%) again had this unique ECG pattern. This time, all 180 were urgently taken to the cath lab. Every single one had a greater than 50% stenosis of the proximal LAD (mean stenosis of 85%).

_______________________________________________________________
T-Wave Abnormalities consistent with Wellens’ Syndrome in V2-3 (may extend to V1-6)
Type A = Biphasic, with initial positivity & terminal negativity (24% of cases)

Type B = Deeply and symmetrically inverted (76% of cases)

Plus:
- Recent history of angina (but Wellens’ ECG pattern is almost always present in pain-free state)
- Normal (or minimal elevation of) serum cardiac markers
- Isoelectric or minimally-elevated ST segment (< 1mm)
- No precordial Q waves
- Preserved precordial R wave progression
________________________________________________________________
Take home points:
It’s all the rage, and for good reason. The HEART score, however, often will not pick up unstable angina. In this case, the score was 2 or 3. One point for age, and 1 or 2 points depending on whether you deem his story moderately or highly suspicious. His initial ECG and troponin were normal.
There are many potential anchoring bias traps. Who wouldn’t rather attribute their pain to that energy drink or chunk of chocolate they ate as the root or what ails them? The left anterior descending (LAD) artery, however, is the ‘Widowmaker’ for good reason. We can’t miss this ECG. Just to make the waters more treacherous, however, is the notion that half the cohort in the original study (and the patient in this case), didn’t manifest a Wellens’ pattern until after they were admitted. A good story, and perhaps point of care ultrasound (POCUS) is all that you may have to go on in the ED; cardiac markers and ECG can, and often will be normal.
This is not a rare entity; 18% and 14% or unstable angina patients in the original and follow up study respectively, had Wellens’ syndrome.
_____________________________________________________________
References:
Zwaan, C de, F W Bär, and H J Wellens. 1982. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. American heart journal, no. 4 Pt 2.
Zwaan, C de, F W Bär, J H Janssen, E C Cheriex, W R Dassen, P Brugada, O C Penn, and H J Wellens. 1989. Angiographic and clinical characteristics of patients with unstable angina showing an ECG pattern indicating critical narrowing of the proximal LAD coronary artery. American heart journal, no. 3.
FOAM Sources:
Dr. Smiths ECG Blog: Wellens’ Syndrome
Life In the Fast Lane: http://lifeinthefastlane.com/ecg-library/wellens-syndrome/
Cardiac Ultrasound: http://www.ultrasoundpodcast.com/tag/cardiac/
PCP Pneumonia
Inspiration:
Jacobi/Montefiore Conference
Edouard Coupet, MD PGY-4
The Case:
Triage: 63 y/o M complains of SOB and cough x 3 days
Nursing Assessment: alert, making grunting noise with breathing
HPI: 63M p/w SOB. Patient notes 2 days of increasing shortness of breath. Also notes a non-productive cough. Denies any pain, but does note subjective fevers and malaise. Denies recent travel.
PMH: HTN, asthma
Meds: amlodipine, albuterol
Physical Exam
T: 101, BP: 137/68, RR: 22, HR: 118, O2: 98% on NRB
General: moderate distress
Skin: WNL
Heart: tachycardic
Lungs: coarse rales
Abd: WNL
Ext: WNL
Labs
Na: 138, Cl: 101, BUN: 32, Glucose: 117
K: 4.9, CO2: 26, Cr: 1.4
WBC: 10.2, Hgb: 8.2, Hct: 24.2, Plt: 306
Emergency Department Course
- O2 sat improved from initial 40% on RA to 90% on non-rebreather. He was then dstarted on non-invasive positive pressure ventilation (BiPAP) 8/5 @ 100% FiO2

- CXR report: diffuse hazy airspace opacity of both lungs, may be due to CHF or pneumonia
- The patient was started on Ceftriaxone and Azithromycin for presumed community acquired pneumonia
- Patient states he was recently tested for HIV and was negative
Three Hours Later
- Patient becomes increasingly hypoxic on NIPPV. Patient was intubated, but course was complicated by multiple desaturations to 70s
- After intubation, patient was noted to be very difficult to bag. Critical care consulted
- “Patient is now intubated and requiring a lot of ventilator support, PEEP 12, and 100% FiO2. Hemodynamically stable. Sedated now. Reason for resp failure likely pneumonia progressing to ARDS. Will cover with Vanc, Zosyn, & Azithromycin. Send urine legionella & pneumococcal antigen. CXR findings could be PCP, send PCP smears. Send HIV study if possible.”
ICU Course
- Patient developed ARDS likely 2/2 PCP and was treated accordingly. He eventually tested positive for HIV and required ECMO and pressors in the ICU. CD4 count was very low
- Patient was deccanulated from ECMO 9 days after presentation and extubated 3 days later. He was started on HAART and PCP prophylaxis per ID recs. He was discharged 32 days after initial presentation
PCP Pneumonia
- Overview:
- Caused by Pneumocystis jiroveci, a fungi, in immunocompromised patients
- This is an AIDS defining illness
- History usually includes shortness of breath, low fever, cough
- Patients with PCP pneumonia can decompensate very quickly and (as in this case) go into ARDS
- How should we diagnose it?
- CXR might show butterfly pattern ie findings in bilateral lungs. These findings are usually interstitial
- PCP pnuemonia increases risk of pneumothorax, which can also be seen on CXR
- CT chest show ground glass opacities
- High LDH (>300 U/I)
- Send sputum cultures to help out your medicine colleagues
- Induced sputum cultures sent to the lab get giemsa and methenamine silver stains
- PCR is also a mode of diagnosis
- How should it be treated?
- Emperic therapy immediately. PCP pneumonia has a very high morbidity and mortality
- First line treatment is TMP-SMX either PO or IV (use IV for more severe cases)
- Trimethoprim 20mg/kg/day and sulphamethoxazole 150mcg/kg/day in 4 divided doses for 21 days
- Alternatives: primaquine + clindamycin, atovaquone, dapsone + trimethoprim
- If patient is HIV positive, steroids will help
- Propylaxis: If CD4 < 200 cells/mm or if HIV positive with history of oropharyngeal candidiasis
References
Coupet E. “M&M Conference: PCP Pneumonia.” Jacobi Medical Center. Jacobi/Montefiore Emergency Medicine Conference. Bronx. Dec 2015. Lecture
Nickson, Chris. “Pneumocystis Jiroveci Pneumonia.” Life in the Fast Lane. Web. 26 Jan. 2016. http://lifeinthefastlane.com/ccc/pneumocystis-jiroveci-pneumonia/
