Follow-up Rounds
1/13/2017
Article inspired by: Dr. Maninder Singh, PGY-3
THE CASE
37 y/o M with no significant PMHx who p/w “allergic reaction” after taking the first dose of PCN 2 hours ago prescribed for Strep Throat diagnosed at an urgent care center. He endorses a sore throat and fever x 2 days but denies any hives or lip/tongue swelling. Denies any prior allergic reactions.
Physical Exam:
- Vitals: BP: 133/76, HR: 107, RR: 15, Temp: 99F, SpO2: 100%
- General: Appears well
- HEENT: NC/AT, PERRL, EOMI, Uvula is midline, Moist mucous membranes, No tonsillar abscesses, Muffled voice, No visible upper oral airway obstruction, Increased saliva production noted; Neck supple, Some lymph node swelling to left precervical nodes
- Cardiovascular: RRR, No murmurs/rubs/gallops
- Chest: CTA b/l, No wheezes/rales/rhonchi
- Abdominal: Soft, NT/ND, BS+ x4
- Extremities: FROM
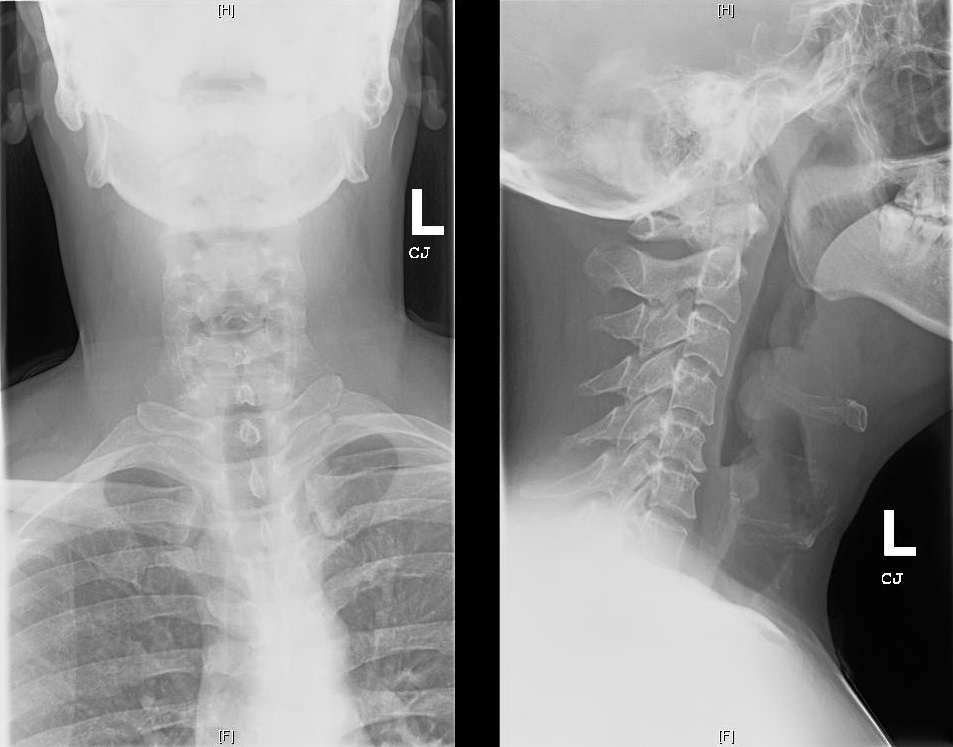
Soft Tissue Neck X-ray:
THE TALK
What is an epiglottis?
- Back wall of the vallecular space below base of tongue
- Infectious epiglottitis = cellulitis of epiglottis
- Progresses to involve entire supraglottic larynx (including aryepiglottic folds and arytenoids) leading to difficulty breathing
Isn’t epiglottitis a pediatric diagnosis?
- Incidence decreased in children since haemophilus influenza vaccination
- Incidence in adults (2006): 1.6 cases per 100,000 adults
- Usually a/w HTN, DM, Substance abuse or immune deficiency
How do I diagnose it?
- Fiberoptic nasal laryngoscopy = gold standard
- Lateral neck x-ray: look for the “thumbprint” sign
- CT neck (if diagnosis unclear)
What do I do if I suspect/diagnose it?
- MANAGE AIRWAY- Be prepared for a cricothyrotomy!
- Have patient sitting up in bed
- Consider prophylactic intubation
- Risk of laryngospasm with scope
- Heliox (mixture of Helium and Oxygen) can be used as a temporizing measure
- Augmentin or Ampicillin-sulbactam (Unasyn) are preferred initial antibiotics
- Consider Vancomycin if patient is critically ill and MRSA a possible etiology
- NSAIDS for pain control
- +/- Steroids for symptomatic relief
This was too long and I didn’t read it- what should I know?
- Patient with sore throat and muffled voice but no obvious signs of upper airway obstruction need further work up
- Have your triple set up ready (direct laryngoscope, video laryngoscope and cricothyroidectomy) and have backup (ENT/Anesthesia) available for a difficult airway
REFERENCES/FURTHER READING:
- Frantz TD, Rasgon BM, Quesenberry CP. Acute Epiglottitis in Adults: Analysis of 129 Cases. 1994;272(17):1358-1360.
- Woods, Charles. “Epiglottitis (supraglottitis): Clinical Features and Diagnosis.” UpToDate, 23 June 2015. Web.
- Rogers, Matt. “Epiglottitis.” Core EM, 26 Aug. 2015. Web.
